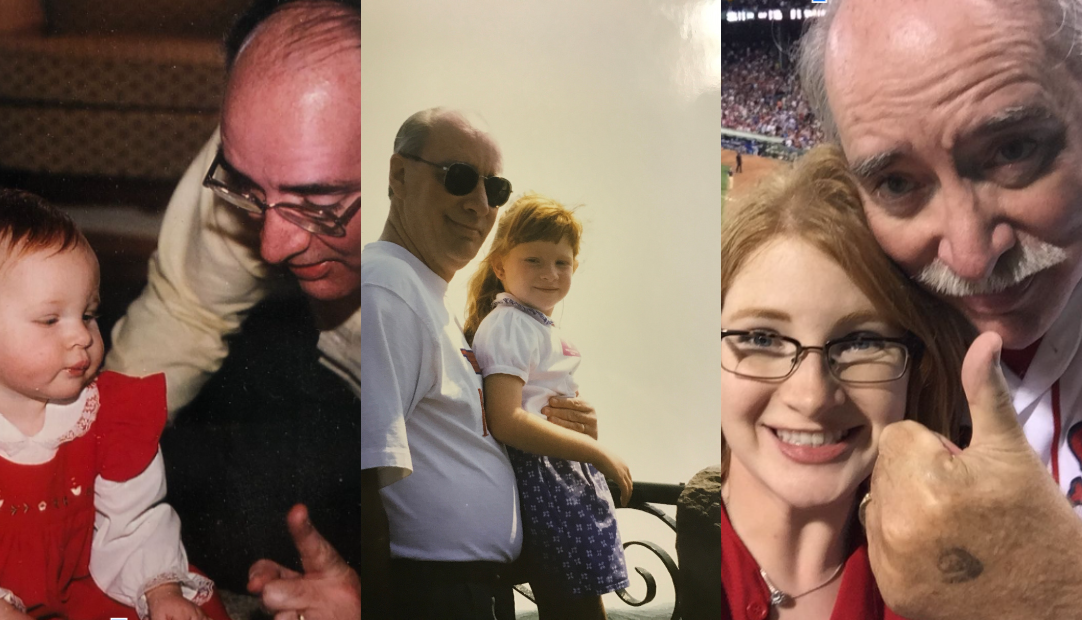
Measuring pancreatic cancer care in moments
Emad Abdelnaby, Senior Vice President, Oncology Franchise Head at Ipsen shares learnings from Dr. Maen Hussein of Florida Cancer Specialists & Research Institute about his approach to treating pancreatic cancer
Nearly 25 years ago, the five-year survival rate for pancreatic cancer was just 5 percent, making it one of the most difficult cancers to treat with the poorest prognosis. Today, pancreatic cancer remains difficult to diagnose early and a hard-to-treat cancer with survival rates hovering around 13 percent. While incremental advancements have been made in the last decade, few patients benefit from this scientific progress. According to the Pancreatic Cancer Action Network, of the 60,000 people newly diagnosed with pancreatic cancer this year, 8,632 people will be able to enjoy life’s moments for five years – more birthdays to celebrate, more family vacations and more memories with friends.
In recent conversations with Dr. Maen Hussein of Florida Cancer Specialists & Research Insitute, our team learned about the progress he’s witnessed firsthand since his fellowship 20 years ago, including a recent FDA-approved regimen for the most advanced form of the disease. He also let us in on the evolution of attitudes and behaviors when it comes to treating people with pancreatic cancer and he shared some best practices he’s learned:
- Establish treatment goals. It’s not a secret that pancreatic cancer carries a poor prognosis, especially when it has spread to other parts of the body. Acknowledge and allow for grief, then create space for patients and families to share their goals and ask questions to make the best decisions for their situation. Oncologists must remember that as goals vary, so should their recommended treatment approach.
- Shared decision-making as a standard. While it’s an overwhelming diagnosis, for people newly diagnosed with pancreatic cancer and their families, it’s extremely important everyone is on the same page. More importantly, this approach puts the patient back into the driver’s seat, which is key for those living with a disease that takes away so much control.
- Simplifying the treatment experience. One approach for oncologists is to approach patients like they are like the manager of a baseball team. Strong managers will have trusted coaches who help them provide comprehensive care and players they can utilize based on the situation. For example, a manager with multiple strong pitchers – or treatment options – will outperform other managers. If the pitcher is ineffective at throwing a strike, they can bring in the second or third pitcher who might be a better fit. Beyond treatment options, using this or a similar analogy is a simplified way to explain utilizing the extended network of care providers who are available to support the patient and their family.
- Normalize second and third opinions. Families shouldn’t feel forced to go with one oncologist’s opinion. Progress needs to continue in this area, but an oncologist shouldn’t get offended when their patients seek a second opinion. Encouraging a second opinion also shows the patient the doctor is comfortable with questions and being challenged.
- Managing side effects. As quality of life is often the backbone topic of patient and caregiver education, oncologists are more proactively discussing possible side effects and how they would be managed. Many treatment side effects are manageable, and a detailed overview ensures families know what to expect. Through this, the foundation of trust is built. Trust leads to more open dialogue, side effect reporting and empowers the family to ask tough questions.
- Overcommunicate. Patients should not be shy about how they’re feeling or questions they may have. Whatever their preferred outreach is, they should engage their full healthcare team as frequently as they desire – don’t let any questions remain unanswered.
In a field where scientific progress has been slow, Dr. Hussein reminds us that a strong doctor-patient relationship also has the potential to shape outcomes and will ultimately create the best possible experience for patients. In tandem with continued innovation, this should make us all optimistic about the future of pancreatic cancer treatment.
Dr. Hussein was compensated for his time by Ipsen.